To be a Medicare Agent's source of information on topics affecting the agent and their business, and most importantly, their clientele, is the intention of this site. Sourced from various means rooted in the health insurance industry - insurance carriers, governmental agencies, and industry news agencies, this is aimed as a resource of varying viewpoints to spark critical thought and discussion. We welcome your contributions.
Friday, August 31, 2018
North Carolina released a much-anticipated...
...Request for Proposals (RFP) for its revamped Medicaid managed
care program. The state expects to move about 70% of its 2,164,945 Medicaid and
CHIP eligibles into managed care plans in late 2019. Aetna Inc., Anthem, Inc.
and Centene Corp. are already said to be interested, according to a report in
AIS's Radar on Medicare Advantage. Contract awards are set to be announced in
February 2019.
Anthem, Walmart Announced MA Partnership
From Health Plan Weekly
On Aug. 20, Anthem, Inc. announced
an arrangement with Walmart Inc. to increase Medicare Advantage (MA) members'
access to over-the-counter (OTC) medicines and health services and products.
It’s a move an expert at KPMG describes as "a natural" fit that may
signal a return to using partnerships to introduce new products, rather than
full-fledged M&A.
Under the Anthem/Walmart program, starting in January 2019, Anthem's MA enrollees will be able to use "OTC plan allowances" to buy OTC medications and health-related items such as pain relievers and first aid supplies at one of Walmart’s 4,700 stores or through its website.
This latest collaboration further emphasizes Anthem's commitment to MA, a program in which the insurer has more than 1 million members, Leerink analyst Ana Gupte, Ph.D., said in an Aug. 20 note. She notes that Anthem's Walmart partnership "stopped short of retail clinics and is also complementary to Anthem’s retail platform, CareMore for Seniors, and complex populations and strengthens Anthem's retail branding, clinical care delivery and distribution in MA."
For major retailers with very large geographic footprints, "there's always been a natural collaboration with the Blues," says Ashraf Shehata, a principal in KPMG's health care life sciences advisory practice.
According to Shehata, the bottom-line question is how to take a long-standing relationship to create new market opportunities. "We've become accustomed to large mergers with large organizations in health care," he says. "This kind of announcement is more along the lines of how health care traditionally was done — through partnerships."
Pharma enters into the equation, too. "The other thing I like about the news is many organizations on the retail side are building generic preferred formularies," Shehata says. "But retailers need to go beyond that with specialty pharmacy [and] be able to leverage retail and health insurance footprints, [which] is happening in these MA partnerships."
Subscribers may read the in-depth article online. Learn more about
subscribing to AIS Health's publications.
Resolving Family Conflicts
Dealing with Alzheimer's can bring out many strong emotions. As the disease progresses, caregiving issues can often ignite or magnify family conflicts. The tips below can help families cope with the situation together.
Tips for families
- Listen to each family member with respect. Coping with a progressive illness, such as Alzheimer's, can be stressful — and not everyone reacts in the same way. Family members may have different opinions. Some relatives may deny what is happening; a long-distance relative may be resented for living far away; or there may be disagreement about financial and care decisions, especially at the end-of-life. These issues are complex and require ongoing discussions. Give everyone an opportunity to share their opinion and avoid blaming or attacking each other, as this will only cause more hurt.
- Discuss caregiving responsibilities. Talk through caregiving roles and responsibilities. Make a list of tasks and include how much time, money and effort may be involved to complete them. Divide tasks according to the family member’s preferences and abilities. Some family members may be hands-on caregivers, responding immediately to issues and organizing resources. Others may be more comfortable with being told to complete specific tasks. Consider setting up an online care calendar to coordinate helpers.
- Continue to talk. Keep the lines of communication open. Schedule regular meetings or conference calls to keep everyone involved up-to-date. Discuss how things are working, reassess the needs of the person with Alzheimer’s, and decide if any changes in responsibilities are needed. Plan for anticipated changes as the disease progresses.
- Cope with changes and loss together. As Alzheimer's progresses and cognitive abilities change, it is normal to experience feelings of loss. Caregivers and family members may want to seek support from others who are dealing with similar situations. Attend a support group in your area or join our ALZConnected online community.
- Seek outside help. If tensions and disagreements are ongoing, you may want to seek help from a trusted third party, such as a spiritual leader, mediator or counselor. Sometimes, an outside perspective can help everyone take a step back and work through the difficult issues. The Alzheimer's Association Helpline (800.272.3900) is staffed with care consultants who can help any time — day or night.
https://alz.org/help-support/resources/resolving-family-conflicts?WT.mc_id=enews2018_08_31&utm_source=enews-aff-172&utm_medium=email&utm_campaign=enews-2018-08-31
CMS provides new flexibility to increase prescription drug choices and strengthen negotiation for Medicare enrollees
 |
|
|
Why CBO won't estimate cost of Bernie Sanders's 'Medicare for all' bill
BY PETER SULLIVAN - 08/29/18
A recent study concluding
that Sen. Bernie Sanders's
(I-Vt.) “Medicare for all” bill would cost $32 trillion has set off a furious
debate over the cost of the plan.
But there's one
estimate that would make an even bigger splash: the score from the nonpartisan
Congressional Budget Office (CBO).
However, it does not
appear that CBO is working on a spending estimate, despite a request from
Sen. John Barrasso (R-Wyo.),
who asked for a cost analysis in September in order to highlight the steep
costs for Medicare for all, also known as single-payer.
Barrasso told The Hill
last week that he doesn’t recall receiving a response from the CBO, suggesting
that his request was not accepted.
The CBO declined to
comment, but former directors said the fact that passing single-payer
legislation is not a priority for the Republican-controlled Congress means the
CBO is unlikely to devote time to scoring the bill.
Doug Elmendorf, a
former CBO director, said the budget scorekeeper is required to provide
estimates only for bills that have made it out of committee and that other
measures it scores are usually the priority of a chairman or ranking member.
Elmendorf, who was CBO
director from 2009 to 2015, noted that “it would take months” for the CBO to
score a bill as complex as single-payer.
“You have to ask yourself,
‘Is there likely to be serious legislative action on it?’ And clearly the
answer to that is no,” said Robert Reischauer, who was CBO director in the
1990s before becoming head of the Urban Institute.
CBO staff are busy
working on more pressing legislation, Reischauer said. “The cost estimating
units are usually operating at full or over capacity,” he said. “It isn’t like
they can accept all requests.”
The release of the
crucial spending analysis is therefore likely to wait until sometime when the
measure is moving through Congress and appears to have a chance of passage.
Republicans have been
pointing to Democratic calls for single-payer as a key rebuttal in this year’s
midterm campaign, part of an effort to push back against Democratic attacks on
GOP bills to repeal ObamaCare. A CBO score before the Nov. 6 elections would
give Republicans a key analysis to point to on the campaign trail.
The releases of CBO
estimates were defining moments in last year’s debate over Republican efforts
to repeal ObamaCare, with the analyses showing that millions of people would
lose coverage under the GOP-backed legislation.
A CBO score would
likely prove pivotal again with Sanders’s single-payer plan, as opponents have
criticized the trillions of dollars in new government spending that would be
required.
Reischauer said that
in this case, “opponents or people who want to embarrass advocates of the plan
want it and nobody else does.”
The release of an
outside study from the right-leaning Mercatus Center at George Mason University
in late July gave a taste of the frenzy that would occur over the release of a
CBO score of single-payer legislation.
Republicans seized on
the Mercatus study’s finding that a single-payer, government-run health
insurance system for all U.S. residents would cost the government an additional
$32 trillion over 10 years.
Speaker Paul Ryan (R-Wis.)
called the cost “absurd.” The Republican National Committee cited the study to
say that Sanders’s plan would “bankrupt taxpayers.”
Barrasso pointed to
the Mercatus study as fodder for the GOP in the absence of a CBO analysis.
“There have been a
number of different reports out there, $32 trillion,” Barrasso said. “It looks
like we have some pretty solid numbers on how expensive it is.”
But Sanders also
touted the report, just a different aspect of it. He pointed to the finding
that total U.S. spending on health care, as opposed to just the government’s
share, would decrease by $2 trillion over 10 years under his legislation.
Elmendorf,
highlighting the consequential decisions that go into any CBO score, said that
the agency might not estimate the bill’s effects on total U.S. health-care
spending, since its core mission is to examine spending by the government.
Leaving that part of the analysis out would deprive Sanders of a key argument
for his bill.
“I think they would do
it if they had enough time,” Elmendorf said.
http://thehill.com/policy/healthcare/404004-why-cbo-wont-estimate-cost-of-bernie-sanderss-medicare-for-all-bill
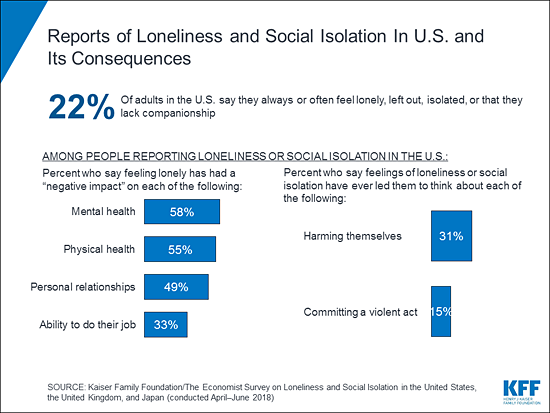
KFF/Economist Survey: One in Five Americans Report Always or Often Feeling Lonely or Socially Isolated, Frequently With Physical, Mental, and Financial Consequences
|
KFF/Economist Survey: One in Five Americans Report Always or Often
Feeling Lonely or Socially Isolated, Frequently With Physical, Mental, and
Financial Consequences
One in five Americans (22%) say they always or
often feel lonely or socially isolated, frequently with serious consequences,
finds a new Kaiser Family Foundation/Economist three-country
survey examining loneliness and social isolation.
Americans who feel lonely or socially isolated
often report negative impacts on their mental (58%) and physical (55%)
health, their personal relationships (49%) and ability to do their job (33%).
Some also say it has led them to think about harming themselves (31%) or
committing a violent act (15%).
The survey also finds that while most Americans
(58%) view the increased use of technology as a major reason why people feel
lonely and socially isolated, those who report feeling lonely or socially
isolated are divided on the impact of social media in particular. About as
many say using social media such as Facebook, Snapchat and Twitter has made
their feelings of loneliness better (31%) and worse (27%).
The survey takes a comprehensive look at the
prevalence, causes and consequences of loneliness and social isolation in the
United States, the United Kingdom and Japan at a time when aging societies
and increasing use of technology is generating concerns about the effects of
loneliness on health. Findings appear in The Economist’s Sept. 1 issue and in
a separate KFF report that looks at people’s views and experiences with
loneliness across the three countries.
Reports of always or often feeling lonely or
socially isolated are similar in the U.S. (22%) and U.K. (23%), compared to 9
percent in Japan.
Other findings include:
The three-country survey is part of a polling
partnership between KFF and The Economist. The poll was designed and analyzed
by survey researchers at KFF in collaboration with The Economist. Each
organization is solely responsible for the content it publishes based on the
survey.
The poll was conducted by telephone from April
through June 2018 among random digit dial telephone (landline and cell phone)
samples of adults in the U.S. (1,003), the U.K. (1,002) and Japan (1,000),
including at least 200 adults in each country who report always or often
feeling lonely or socially isolated.
The margin of sampling error is plus or minus 3
percentage points for the U.S. results and plus or minus 4 percentage points
for results for the U.K. and Japan. For results based on subgroups, the
margin of sampling error may be higher.
Filling
the need for trusted information on national health issues, the Kaiser Family Foundation is a nonprofit
organization based in San Francisco, California.
|
|
|
|
June 2018 monthly report on state Medicaid and Children's Health Insurance Program (CHIP) eligibility and enrollment data.
|
Outreach Strategies to Help Your Organization Reach Uninsured Families Living in Rural Communities
Outreach
Strategies to Help Your Organization Reach
Uninsured
Families Living in Rural Communities
Children in rural communities are disproportionately uninsured
compared to their counterparts in urban and suburban locations across the
country, and for those who have coverage in rural communities, they are more
likely to rely on Medicaid and the Children’s Health Insurance Program
(CHIP).
With nearly 60 million individuals currently living in rural areas, it’s more important than ever to engage with these communities. By working closely with local organizations, small businesses, and health providers, your organization can help eligible families gain access to coverage. The Connecting Kids to Coverage National Campaign’s recent webinar explored ways organizations can reach eligible families where they work, play, and pray and enroll children in Medicaid and CHIP. We also shared best practices and proven tips to make rural health outreach and enrollment efforts a success.
Campaign in Action
The CMS Office of Minority Health (OMH) works with local and federal partners to eliminate health disparities while improving the health of all minority populations through its health equity initiatives. Studies show that minority populations in rural areas tend to be younger and are less likely to report being in good health than their non-Hispanic white counterparts. Together with OMH, the Consortium for Medicaid & Children’s Health Operations launched a rural health strategy to improve access and quality of care specifically for rural Americans. By leveraging local and community partnerships, the Consortium empowers patients in rural communities to make independent decisions about their healthcare. The U.S. Department of Health & Human Services’ Office of the Assistant Secretary for Health (OASH) is focused on increasing the nation’s investment in health and science to advance health equity and improve the health of all people. OASH has 10 regional health offices across the nation that are managed by 10 different regional administrators. OASH’s experience working within Region X, a large territory that covers Idaho, Oregon, Washington, and Alaska, proved to be a helpful lesson in how strong community partnerships can work for any organization. With limited resources and a staff stationed in Seattle, the regional office formed partnerships with state and local health departments, various health systems, and community-based organizations to successfully connect families across all states in the region to health coverage. While partner relationships are very important, it is also essential to form meaningful relationships directly with families. The Native American Rehabilitation Association of the Northwest (NARA) has provided physical and mental health services, including dental clinics, wellness health centers, and drug and alcohol treatment programs, to American Indians and Alaska Natives (AIs/ANs) in rural communities since 1970. NARA specializes in boosting enrollment in areas that are geographically isolated and lack adequate healthcare facilities and staff. The organization works to combat the cultural factors that deter rural families from enrolling in coverage, such as feelings of distrust towards outsiders and general misconceptions about the services provided through Indian Health Service. Staying up-to-date on key rural health issues helps make outreach efforts relevant to the families and organizations you serve. Rural Health Information Hub (RHIhub) is an online guide to improving health within rural communities and provides current resources and tools that can help your organization learn more about rural health-specific needs. RHIhub features a selection of different evidence-based online toolkits, including resources specifically designed for rural community health workers, oral health and health literacy.
New Rural Health Initiative Page and Campaign Materials
The Connecting Kids to Coverage National Campaign: Reaching Rural Communities web page contains resources specific for conducting rural health outreach, including the “5 Ways to Conduct Outreach in Rural Communities” tip sheet. This tip sheet contains tips for identifying eligible rural families, partnering with local organizations and small businesses, and leveraging partnerships with health providers. And the “Connecting Kids to Coverage: Kentucky” outreach video demonstrates how health centers, like Mountain Comprehensive Health Corporation, are working to expand access to health care in rural communities. The Campaign’s Outreach Tool Library also features ready-to-use tools like message guides, templates, and resource links, and offers social media graphics for Facebook and Twitter
We want to hear your success story!
Does your organization use targeted outreach strategies to enroll rural families in Medicaid and CHIP? If so, we'd like to learn how your organization is connecting kids to coverage! Share details with the Campaign via email at ConnectingKids@cms.hhs.gov or on Twitter using the hashtags #Enroll365 and #KidsEnroll.
Stay Connected with the Campaign
The Connecting Kids to Coverage National Campaign Notes
eNewsletter is distributed throughout the year and provides updates on
Campaign activities. If a friend or colleague forwarded this email to
you, sign up to receive this eNewsletter
directly to your inbox.
|
|
|
The Centers for Medicate &
Medicaid Services (CMS)
To
contact CMS, please visit our contact us page.
|
Prevent osteoporosis
Prevent osteoporosis
|
|
|
Many
people don’t know they have osteoporosis until they break a bone. Did you
know Medicare can help you prevent or detect osteoporosis at an early stage,
when treatment works best?
Talk to your doctor
about getting a bone mass
measurement (bone density). If you’re at risk, Medicare Part B covers this test once
every 24 months (more often if medically necessary) at no cost to you, when
your doctor or other qualified provider orders it.
You can take steps to make your bones stronger and healthier, no matter your age.Talk to your doctor, and visit Medicare.gov to find out how Medicare can help protect your bones.
Sincerely,
The
Medicare Team
|
Wednesday, August 29, 2018
August 23, 2018
Associated Press August 23, 2018
WASHINGTON (AP)
— A congressional watchdog said the Trump administration needs to step up its
management of sign-up for former President Barack Obama's health care
law after mixed results last year in the throes of a
failed GOP effort to repeal it.
The report due out
Thursday from the Government Accountability Office is likely to add
to Democrats' election-year narrative that the administration
actively undermined "Obamacare" without regard for the consequences
to consumers.
The nonpartisan
Government Accountability Office was more nuanced. On one hand, it found
problems with consumer counseling and advertising and recommended such basic
fixes as setting enrollment targets. But it also credited administration
actions that did help people enroll, such as a more reliable HealthCare.gov website
and reduced call center wait times.
Sign-ups for 2019
begin this November.
A copy of the
report from the investigative agency for Congress was provided to The
Associated Press.
It found that:
— The Health
and Human Services Department under Trump broke with its own previous
practice by failing to set enrollment targets for HealthCare.govlast
year. The watchdog recommended that HHS resume setting goals, a standard
management tool for government agencies. Without setting numeric goals, HHS
won't be able to measure whether it is meeting "its current objective of
improving Americans' access to health care," the report said. The
administration responded that it does not believe such targets are relevant.
— HHS used
"problematic" and "unreliable" data to justify a 40 percent
cut in funding for enrollment counseling programs known as Navigators. HHS
responded that it's making changes to how those counseling programs are
evaluated. But it has cut funding again, by about 70 percent.
— When HHS slashed
money for open-enrollment advertising by 90 percent overall, officials said
they were doing away with wasteful spending. But an internal study by the
department had actually found paid television ads were one of the most
effective ways to enroll consumers. The budget for TV ads went from $26.6
million in the Obama administration's final year to zero under
President Donald Trump.
"This
independent and nonpartisan GAO report confirms that the Trump administration's
sabotage of our health care system is driving up costs for consumers and
leaving more Americans without health insurance," said a statement from a
group of Democratic lawmakers led by Rep. Frank Pallone of New
Jersey.
HHS said in a
statement that the 2018 enrollment season was the "most cost-effective and
successful experience" for consumers, citing a 90 percent customer
satisfaction rate with the HealthCare.gov call center.
Republicans' drive
to "repeal and replace" the health care law stalled in
the Senate last year, and the Trump administration instead found
itself having to run a program the president repeatedly branded a
"disaster."
The watchdog found
that sign-ups in the 39 states served by HHS through the federal HealthCare.gov website
dipped by 5 percent last year, while states running their own enrollment effort
maintained their sign-up levels. A total of 11.7 million people enrolled for
2018 coverage, with about 85 percent receiving subsidies to help pay their
premiums.
The report
validated a longtime Republican criticism that high premiums discourage
consumers from signing up for coverage. But it also found that Trump contributed
to premium increases for 2018 by canceling payments that reimburse insurers for
lower deductibles and copays provided to low-income people. That forced the
carriers to jack up rates.
"Substantial
increases" in premiums triggered by Trump cut both ways, the watchdog
found. People with modest incomes entitled to subsidies got more financial aid
from the government, and their coverage became more affordable. But solid
middle-class customers paying full premiums were priced out of the market.
Subscribe to:
Posts (Atom)