|
Just Released
|
|
|
50-State Survey Finds Medicaid Enrollment Growth Slowing, with an
Uptick in Spending Growth Driven by Provider Rate Increases and Rising Costs
for Rx Drugs and Long-Term Care
Several
States Are Seeking to Restrict Medicaid Eligibility through Waivers
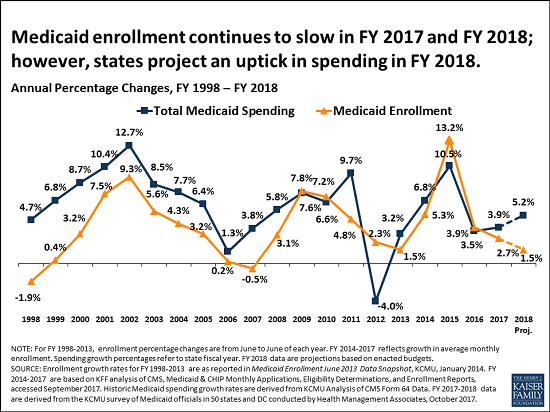
Medicaid enrollment growth slowed to 2.7 percent
in state fiscal year 2017, down from 3.9 percent the prior year and far off
the peak of 13.2 percent in 2015 that followed implementation of the
Affordable Care Act’s (ACA) Medicaid expansion, according to a new survey from the Kaiser Family Foundation. Findings
of Kaiser’s 17th annual 50-state survey of Medicaid directors
across the country suggest the slowdown in enrollment growth may be
attributable to the tapering of new ACA-related Medicaid enrollment, a stable
economy, and states’ processing of delayed eligibility redeterminations.
At the same time, total Medicaid spending grew by
3.9 percent in state FY 2017 and states project it will grow by 5.2 percent
in state FY 2018, down from 10.5 percent growth in state FY 2015 after
implementation of the ACA. Major drivers of spending growth include rising
costs of prescription drugs and long-term care services and supports, and
increases in payment rates for most provider groups.
State Medicaid spending grew by 3.5 percent in
state FY 2017 and states project it will grow by 6 percent in state FY 2018,
in part because the 32 expansion states are now paying a share of ACA
Medicaid expansion costs after several years in which the federal government
footed the entire bill. The Medicaid expansion states began paying 5 percent
of expansion costs in January 2017, midway through state FY 2017. State FY
2018 is the first full budget year that states will have to cover some
expansion costs, with states’ share rising to 6 percent in January. In
addition, some states are experiencing a decrease in the formula-driven federal
match rate for the traditional Medicaid population that can result in faster
state spending growth.
The survey findings come at a time of uncertainty
for Medicaid and state budgets. Forty-eight states assumed continuation of
federal Children’s Health Insurance Program (CHIP) funding in their state FY
2018 budgets; that money expired in September and 11 states report they will
exhaust federal funding by the end of 2017 if Congress does not reauthorize
it. Nearly two-thirds of states also did not budget for reductions in
Medicaid disproportionate share (DSH) payments. Congress had delayed those
cuts, originally scheduled for federal FY 2014, to October 2017. States
were busy preparing estimates of the effects of repeal and replace
legislation and many assumed that Congress would act to reauthorize CHIP and
potentially delay DSH reductions further into the future.
Medicaid
waivers
In an emerging trend, several states are seeking
approval to implement Medicaid eligibility restrictions through pending
Section 1115 waivers. Proposed restrictions include work requirements (AR,
IN, KY, ME, UT, WI); time limits on coverage (ME, UT, WI); eliminating
retroactive eligibility (AR, IA, ME, UT); ending Medicaid expansion coverage
for people with incomes above the poverty level while maintaining the enhanced
federal matching rate for the remaining expansion population (AR, MA); and
drug screening and testing (WI). Although these waivers are pending, several
states plan to implement some of the proposed restrictions in state FY 2018.
Opioid
concerns
As public concern rises about opioid addiction and
overdose deaths, more state Medicaid programs are adopting Centers for
Disease Control guidelines for the prescribing of opioids, and nearly all
have various fee-for-service pharmacy management strategies targeted at
opioid harm reduction. Forty-six states reported that naloxone, an opioid
overdose antidote, was available without prior authorization.
Other survey findings include:
These and other findings from the 50-state survey,
conducted by analysts at the Foundation and Health Management Associates,
were discussed today at a briefing held jointly by the Foundation and the
National Association of Medicaid Directors (NAMD). The following new reports
are available:
An archived webcast of the briefing, as well as copies of
presentation slides and other materials, will be available on kff.org later
today.
Filling
the need for trusted information on national health issues, the Kaiser Family Foundation is a nonprofit
organization based in Menlo Park, California.
|
|
To be a Medicare Agent's source of information on topics affecting the agent and their business, and most importantly, their clientele, is the intention of this site. Sourced from various means rooted in the health insurance industry - insurance carriers, governmental agencies, and industry news agencies, this is aimed as a resource of varying viewpoints to spark critical thought and discussion. We welcome your contributions.
Tuesday, October 24, 2017
50-State Survey Finds Medicaid Enrollment Growth Slowing
Subscribe to:
Post Comments (Atom)
No comments:
Post a Comment