|
Just Released
|
||
|
As All States Streamline Medicaid
Enrollment and Renewal Processes, New Eligibility Requirements Pursued By
Some States Could Increase Administrative Complexity and Reduce Coverage
Annual 50-state Survey Also Finds Eligibility
Levels Remain Very Low in Non-expansion States
All states continue to implement new Medicaid
enrollment and renewal processes that can connect individuals to coverage
more quickly and reduce administrative paperwork, finds KFF’s annual 50-state survey of Medicaid eligibility
and enrollment policies. At the same time, some states are pursuing new
eligibility requirements, such as work requirements and monthly premiums,
that would push in the opposite direction, increasing the complexity of
enrollment processes and potentially reducing coverage.
The ongoing technological and enrollment process
upgrades required of all states under the Affordable Care Act mean that this
year, for the first time, individuals can apply online for Medicaid in all
states, the survey finds. Moreover, 46 states can complete Medicaid
eligibility determinations within 24 hours, and 46 can perform automated
renewals.
While all states have streamlined enrollment and
renewal processes, not all states have expanded coverage to adults under the
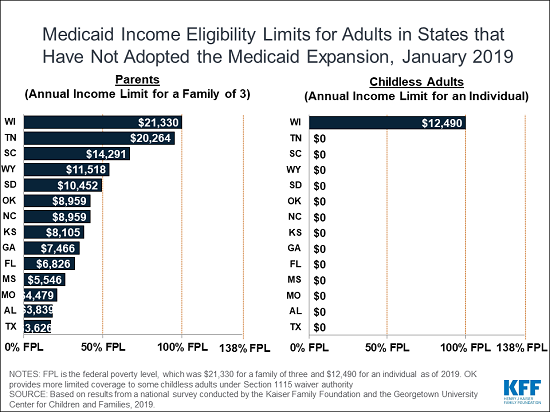
ACA. In the 14 states that had not adopted the Medicaid expansion,
eligibility for parents and other adults remained very limited. The median
eligibility level for parents in these states was 40 percent of poverty ($8,532
per year for a family of three). In Texas, eligibility is limited to 17
percent of the federal poverty level or less than $4,000 per year for a
parent in a family of three. Other adults were ineligible regardless of
income in all these states except Wisconsin.
Separately, some states are seeking and
implementing new eligibility rules, often through waivers. Such measures
include imposing work requirements, mandatory health risk assessments,
charging monthly premiums, eliminating retroactive eligibility, delaying
coverage until the first premium payment and locking enrollees out of
coverage if they fail to pay premiums or renew their eligibility on time.
Many of these measures require complex and costly documentation and
administrative efforts, which can raise barriers to coverage and contribute
to coverage losses, in contrast to the push for increased coverage and
streamlined enrollment processes under the ACA.
The 17th annual survey provides a
comprehensive look at Medicaid and CHIP eligibility, enrollment, renewal,
premium and cost sharing policies for each state as of January 2019. These
annual surveys will continue to track future policy changes.
The full survey, Medicaid and CHIP Eligibility, Enrollment, Renewal, and Cost Sharing
Policies as of January 2019: Findings from a 50-State Survey,
conducted with Georgetown University’s Center for Children and Families, as
well as reports from previous years, can be found on KFF.org.
Filling the need for trusted information on
national health issues, the Kaiser Family Foundation is a
nonprofit organization based in San Francisco, California.
|
||
|
|
||
To be a Medicare Agent's source of information on topics affecting the agent and their business, and most importantly, their clientele, is the intention of this site. Sourced from various means rooted in the health insurance industry - insurance carriers, governmental agencies, and industry news agencies, this is aimed as a resource of varying viewpoints to spark critical thought and discussion. We welcome your contributions.
Wednesday, March 27, 2019
As All States Streamline Medicaid Enrollment and Renewal Processes, New Eligibility Requirements Pursued By Some States Could Increase Administrative Complexity and Reduce Coverage
Subscribe to:
Post Comments (Atom)

No comments:
Post a Comment