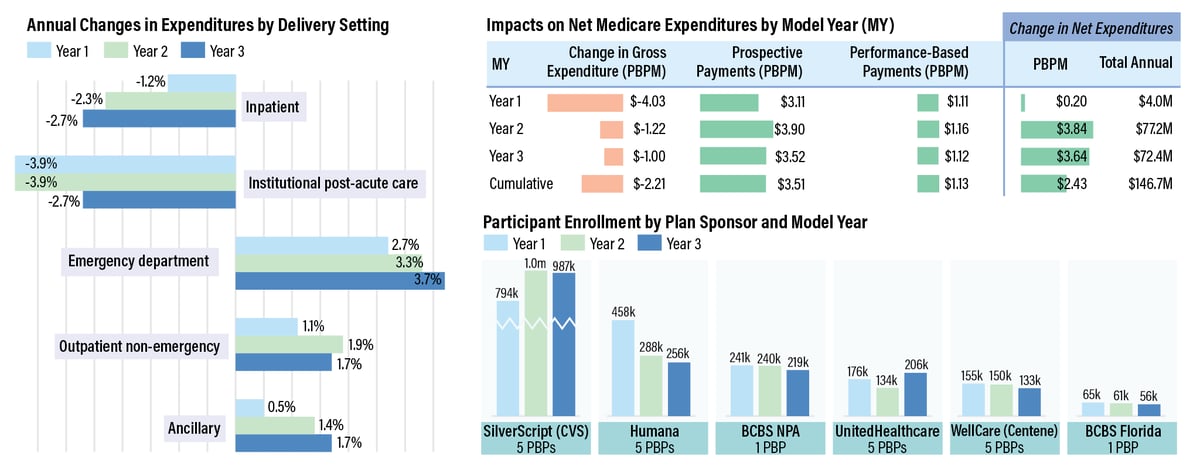
The CMS Center for Medicare and Medicaid Innovation's Part D
Enhanced Medication Therapy Management (MTM) Model did not show significant
savings in its first three years, according to an August 2021 evaluation
conducted by Acumen, LLC. In each year, CMS's combined payments to
participating plan sponsors were larger than the decreases in Medicare Parts A
and B spending, offsetting the cumulative savings of $2.21 per beneficiary per
month (PBPM) over the course of the program. While the cost of care delivery in
inpatient and institutional post-acute settings decreased, suggesting that the
model may help reduce hospital readmissions, an unexpected increase in spending
and utilization of emergency room services neutralized the financial impact.
And because beneficiaries were encouraged to make follow-up visits to their
prescribers, this may explain the increased spending in outpatient and
ancillary settings. Overall, while the demonstration did correlate to
improvement in some areas, CMS said it likely won't repeat this type of
financial model in the future.
SOURCE: CMS, "Evaluation of the Part D Enhanced Medication Therapy Management (MTM) Model: Third Evaluation Report," submitted by Acumen, LLC to the Center for Medicare and Medicaid Innovation, August 2021. Visit https://bit.ly/3ALOCO5.
No comments:
Post a Comment