|
Just Released
|
||
|
50-State Survey Finds Flat Medicaid Enrollment Tied to a Stronger
Economy and New Eligibility Systems
Average Spending Growth Outpaces
Enrollment Due to Pressure from Rising Costs for Prescription Drugs and
Long-Term Services and Supports
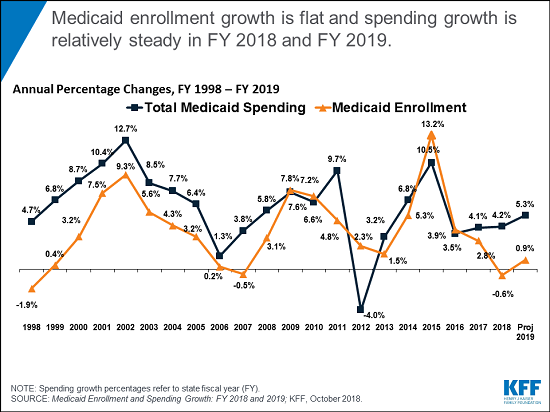
For the first time in
a decade, states are reporting no overall growth in Medicaid enrollment last
year and expecting minimal growth this year amid a stronger economy, a new Kaiser Family Foundation survey finds.
The 18th annual
50-state survey of Medicaid directors reveals that enrollment was flat in
state fiscal year (FY) 2018 (down an average 0.6 percent), and states are
budgeting for minimal increases during FY 2019 (up an average 0.9 percent).
States largely
attribute the enrollment slowdown to a strengthening economy, resulting in
fewer new low-income people qualifying for Medicaid. Some states also cited
new efforts and systems to verify enrollees’ continued eligibility for the
program as a factor.
At the same time,
average combined federal and state Medicaid spending grew by 4.2 percent in
FY 2018, similar to the previous year’s growth, and states project an average
5.3 percent increase in Medicaid spending in FY 2019.
The gap between
enrollment and spending growth in part reflects lower enrollment growth for
children and adults, who are relatively inexpensive to cover, compared to
seniors and people with disabilities, who have more expensive needs. Other
factors include:
In FY 2018, state spending grew slightly faster
(4.9 percent) than total Medicaid spending (4.2 percent), as this was the
first full state fiscal year that states were responsible for a share of the
Affordable Care Act’s Medicaid expansion. Despite a modest increase in the
state share of the expansion costs, states’ adopted budgets for FY 2019
anticipate that state spending for Medicaid will grow more slowly than total
Medicaid spending (3.5 percent compared to 5.3 percent).
The annual survey provides an in-depth,
state-specific examination of changes taking place in Medicaid
programs. Some common themes include:
Changing
eligibility. In response to the Trump administration’s
encouragement, a growing number of states are pursuing federal waivers to add
work requirements to Medicaid that are likely to result in enrollment
declines. In FY 2019, eight states are planning to implement work or
community engagement requirements, though some still are awaiting federal
approval to implement. Three states (Idaho, Nebraska and Utah) could
adopt the ACA Medicaid expansion through November 2018 ballot initiatives.
Controlling drug costs. In FY 2018, 22 states reported new or enhanced pharmacy
cost-containment initiatives, and 19 plan to implement such initiatives in FY
2019. These changes often aim to boost rebate revenue or implement new prior
authorization requirements, step therapy or other utilization controls.
Focusing on quality and value. States are continuing to focus on delivery system
changes and managed care requirements to improve quality, outcomes and
value. Nearly all states with comprehensive, risk-based managed care
reported various quality initiatives. An increasing number of states (23 in
FY 2018) are setting targets for alternative provider payment arrangements in
managed care contracts. Many states
encourage or require managed care organizations to screen enrollees for
social needs, and about one-third of all states report initiatives for FY
2018 and FY 2019 that address social determinants of health outside of
managed care.
Reducing opioid risks. All 50 states and the District of Columbia reported at
least one pharmacy-management strategy aimed at addressing the opioid
epidemic, including quantity limits on opioid drugs (50 states), clinical
criteria claims system edits (48 states), step therapy (39 states) and other
prior authorization requirements (44 states). In addition, most states that
use managed care to deliver drug benefits require those organizations to
follow some or all of these opioid policies.
Expanding benefits. In FY 2018, 19 states expanded their Medicaid
benefits, and 24 plan to do so in FY 2019. The most common benefit
enhancements involve substance use and mental health services, including
waivers to allow Medicaid to pay for care in institutions for mental disease.
The findings are
included in two reports:
The 50-state survey,
conducted by analysts at KFF and Health Management Associates in partnership
with the National Association of Medicaid Directors (NAMD), will be discussed
today at a briefing held jointly by KFF and NAMD.
Filling
the need for trusted information on national health issues, KFF (The Kaiser Family Foundation) is a nonprofit
organization based in San Francisco, California.
|
||
|
||
To be a Medicare Agent's source of information on topics affecting the agent and their business, and most importantly, their clientele, is the intention of this site. Sourced from various means rooted in the health insurance industry - insurance carriers, governmental agencies, and industry news agencies, this is aimed as a resource of varying viewpoints to spark critical thought and discussion. We welcome your contributions.
Thursday, October 25, 2018
50-State Survey Finds Flat Medicaid Enrollment Tied to a Stronger Economy and New Eligibility Systems
Subscribe to:
Post Comments (Atom)

No comments:
Post a Comment