States are moving to better
address social determinants of health (SDOH) and improve health equity in their
Medicaid programs, and they’re asking MCOs to drive the change, according to an
analysis of recent requests for proposals (RFPs) from advocacy group Together
for Better Medicaid. The report identified RFPs from 10 states that have
extensive SDOH and equity-based requirements for MCOs, from member screenings
and staff training to close collaboration with community-based organizations
(CBOs). Meanwhile, Medicaid enrollment has surged in all 10 states amid the
COVID-19 pandemic. National Medicaid enrollment climbed 18.4% from March 2020
to December 2021, according to AIS’s Directory of Health Plans. See an overview
of the most common SDOH requirements and the 10 states’ recent enrollment
patterns below.
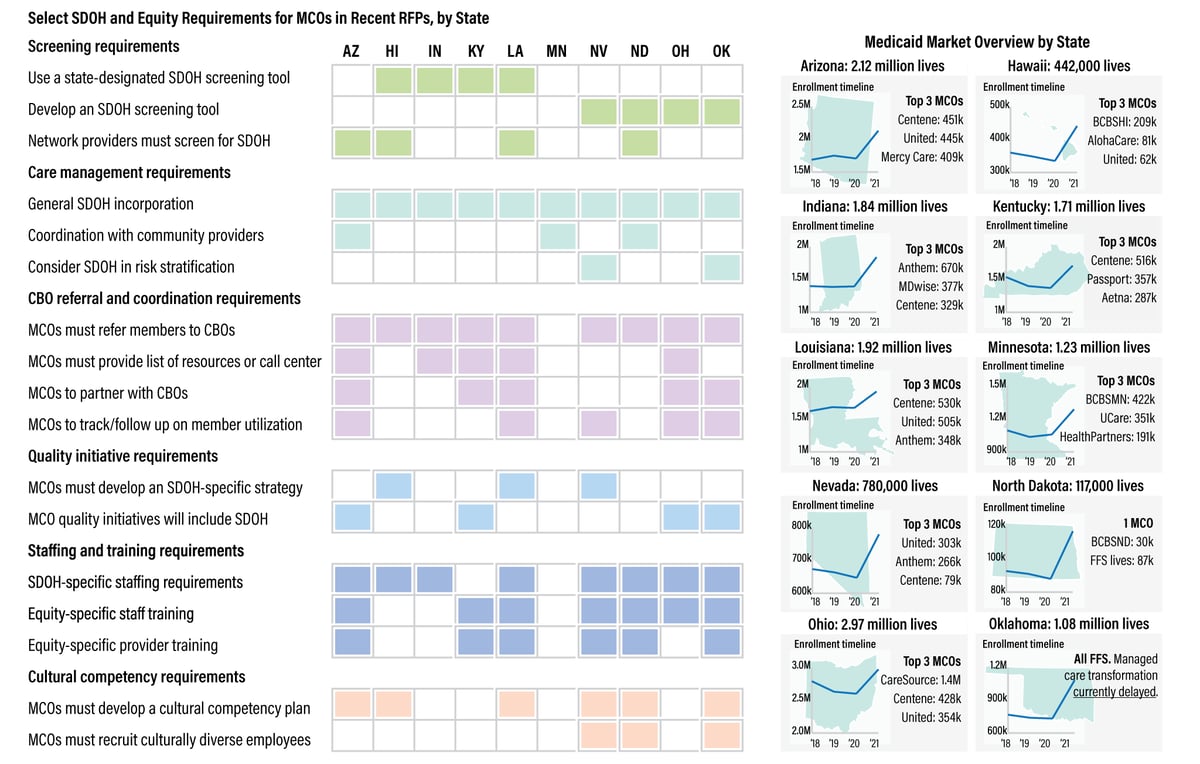
SOURCE: DHP, AIS’s Directory of Health Plans; “Medicaid Managed Care: Strategies
to Address Social Determinants of Health and Health Equity,” prepared for
Together for Better Medicaid by Health Management Associates (HMA), December
2021.
This comment has been removed by a blog administrator.
ReplyDelete