The
United States is facing the biggest surge of COVID-19 cases to date. According
to the Centers for Disease Control and Prevention (CDC), on Tuesday, January
11, there were 797,216 new cases of the disease.[1] To put this into context, during the
summer of 2020, the peak number of new COVID cases per day was 77,000 – a more
than tenfold increase since that time.[2]
Cases are also geographically widespread, with 99.13 percent of the counties in
the U.S. experiencing “high” levels of community transmission of COVID-19.[3] The CDC measures
transmission level by examining the total new cases of COVID-19 infections
reported over the past 7 days and the percent of positive COVID tests for the
county over the past 7 days.[4]
The higher number of new cases and higher percent positivity correspond to
higher levels of community transmission.
In
Connecticut, for example, every county is rated with a high transmission level.
While 79.4 percent of the state’s population of five-year-olds and over are
vaccinated, Connecticut’s Department of Public Health is reporting a 24 percent
positivity rate.[5]
Furthermore, 82 percent of hospitals beds in the state are filled, and over a
quarter of them are being used for COVID-19 patients. Connecticut’s utilization
statistics are slightly higher than the national average of 79.15 percent of
beds being filled, and just over one-fifth being used for those with COVID-19.[6]
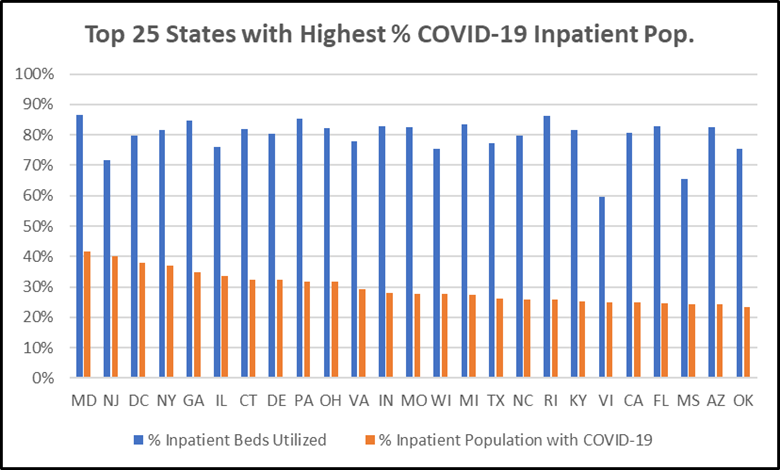
The
Center for Medicare Advocacy analyzed state-aggregated data for hospital
utilization provided by the Department of Health & Human Services (HHS).[7] We highlight the top
25 states with the highest percent of inpatient population with suspected or
confirmed COVID-19. Maryland ranked highest, with 42 percent of hospital
patients having or suspected to have COVID and inpatient utilization at 87
percent. Connecticut ranks 7th, with 32 percent of hospital patients
having or suspected to have COVID-19.
Exacerbating
this strain is the fact that hospitals are facing critical staff shortages. All
but five states, along with Puerto Rico, the Virgin Islands, and American
Samoa, reported hospitals with critical staff shortages.[8]
___________________
[1] CDC. Trends in Number of COVID-19 Cases and
Deaths in the US Reported to CDC, by State/Territory. Centers for
Disease Control and Prevention. (Updated January 12, 2022). Available at: https://covid.cdc.gov/covid-data-tracker/#trends_dailycases
[2] CDC. Trends in Number of COVID-19 Cases and
Deaths in the US Reported to CDC, by State/Territory. Centers for
Disease Control and Prevention. (Updated January 12, 2022). Available at: https://covid.cdc.gov/covid-data-tracker/#trends_dailycases
[3] CDC. Covid-19 County Check Tool.
Centers for Disease Control and Prevention. (September 30, 2021). Available at:
https://www.cdc.gov/coronavirus/2019-ncov/more/aboutcovidcountycheck/index.html
[4] CDC. Covid-19 County Check Tool.
Centers for Disease Control and Prevention. (September 30, 2021). Available at:
https://www.cdc.gov/coronavirus/2019-ncov/more/aboutcovidcountycheck/index.html
[5] CT.gov. Connecticut COVID-19 data tracker.
CT.gov. (Updated January 11, 2022). Available at: https://portal.ct.gov/Coronavirus/COVID-19-Data-Tracker
[6] HHS. Hospital Utilization. HHS
Protect Public Data Hub. (Updated January 12, 2022). Available at: https://protect-public.hhs.gov/pages/hospital-utilization
[7] U.S. Department of
Health & Human Services. Covid-19
reported patient impact and hospital capacity by State.
HealthData.gov. (Updated January 12, 2022). Available at: https://healthdata.gov/dataset/COVID-19-Reported-Patient-Impact-and-Hospital-Capa/6xf2-c3ie
[8] HHS. Hospital Utilization. HHS
Protect Public Data Hub. (Updated January 12, 2022). Available at: https://protect-public.hhs.gov/pages/hospital-utilization
This comment has been removed by a blog administrator.
ReplyDelete