Most older adults in the U.S.
have been diagnosed with one or more chronic illnesses, and managing these
conditions presents a significant cost burden, according to a January study in
JAMA Internal Medicine. The authors studied eight of the most common chronic
conditions, both as single disease states and in clusters, and determined
hypothetical annual out-of-pocket (OOP) costs for individual seniors enrolled
in Medicare Advantage-Prescription Drug plans and Standalone Part D plans in
2009 and 2019. While annual costs for many of the conditions dropped, likely
due to the availability of new generic drugs, OOP costs for atrial
fibrillation, type 2 diabetes and heart failure skyrocketed. This was
attributed to the introduction of brand-name therapies without generic
alternatives that received clinical guideline recommendations. To remedy this,
study authors urged Congress to act on drug pricing reforms, including allowing
Medicare to negotiate list prices and cap annual OOP costs for seniors.
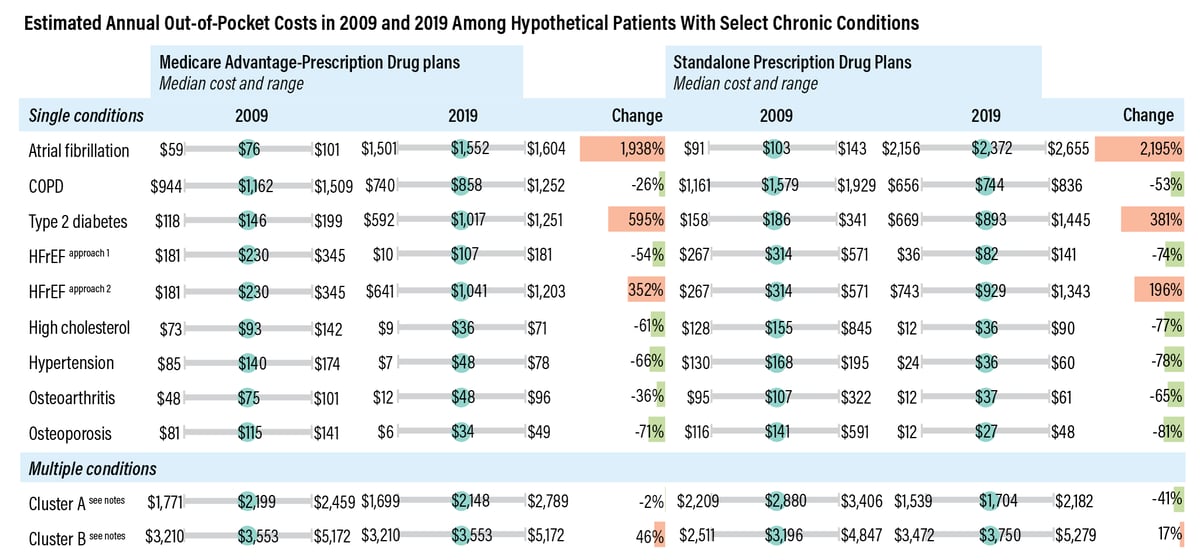
NOTES: COPD=chronic obstructive pulmonary disease; HFrEF=heart
failure with reduced ejection fraction. Out-of-pocket costs were inflation
adjusted to 2019 dollars. HFrEF Approach 1 assumed the patient was prescribed
an angiotensin-converting enzyme inhibitor or angiotensin receptor blocker, an
evidence-based beta blocker, and an aldosterone antagonist in 2019. HFrEF
Approach 2 assumed the patient was prescribed an angiotensin receptor
neprilysin inhibitor (sacubitril-valsartan), an evidence-based beta blocker,
and an aldosterone antagonist in 2019. Cluster A conditions include COPD, type
2 diabetes, hypertension, osteoarthritis and osteoporosis. Cluster B conditions
include atrial fibrillation, COPD, type 2 diabetes, HFrEF (approach 1), high
cholesterol, hypertension, osteoarthritis and osteoporosis.
SOURCE: “Assessment of Hypothetical Out-of-Pocket Costs of
Guideline-Recommended Medications for the Treatment of Older Adults With
Multiple Chronic Conditions, 2009 and 2019,” JAMA, Jan. 4, 2022.
From Radar on Medicare
Advantage
No comments:
Post a Comment