More
than two months ago, on August 14, 2020, the Centers for Medicare &
Medicaid Services (CMS) reported that it had cited more than 180 “immediate
jeopardy” level deficiencies for infection prevention and control at nursing facilities,
triple the rate from 2019, and that it had imposed civil money penalties
exceeding $10 million for the deficiencies.[1] CMS acknowledged in a call with
nursing home residents’ advocates on August 19 that the data reported on August
14 were available only in an internal CMS database, not on its two
publicly-reported databases.
The
Center for Medicare Advocacy (Center) analyzed data on CMS’s Quality,
Certification and Oversight Reports (QCOR) database, which CMS updates weekly,
and reported on August 20, 2020 that QCOR data showed far fewer immediate
jeopardy deficiencies in infection control than CMS reported.[2]
Now,
two months later, the Center has analyzed QCOR data and again found inaccuracies
in the database and far fewer than 180 immediate jeopardy infection control
deficiencies.
|
Why do
infection control deficiencies matter? Failure
to address infection control deficiencies effectively and permanently can
result in residents’ deaths. Andbe Home, a Kansas nursing facility, was
cited with a no-harm infection control deficiency at its standard survey on
December 18, 2018. The facility was cited with an immediate jeopardy
deficiency in infection control on May 20, 2020 (as shown on both QCOR and
CMS’s September 30, 2020 data release). Although the facility claimed
to have promptly corrected the deficiencies, as of October 21, 2020, all 62
residents at the facility and many staff were infected with coronavirus and
10 residents had died.[1] QCOR does not reflect that the facility
received a fine for its infection control deficiency (as of October 22). |
On
October 9, the Center searched QCOR for infection prevention and control
deficiencies (F-880), at the immediate jeopardy level that had been cited since
January 2020. QCOR identified 384 deficiencies as meeting these
criteria. Analyzing a 20% sample of the data (59 of the 294 facilities),[3] the Center found:
- 11 of the 59 facilities did not have any survey in calendar
year (CY) 2020
- 23 of the 59 nursing facilities had a survey in CY 2020, but
they were not cited with an infection control deficiency
- Only 29 infection control deficiencies were cited in CY 2020
- Only 25 nursing facilities cited 29 infection control
deficiencies in CY 2020
Eighteen
of the 29 infection prevention and control deficiencies (62%) identified in
QCOR were cited at the immediate jeopardy level. The immediate jeopardy
deficiencies were cited in 18 facilities, several of which were also cited with
a non-immediate jeopardy deficiency in infection control.
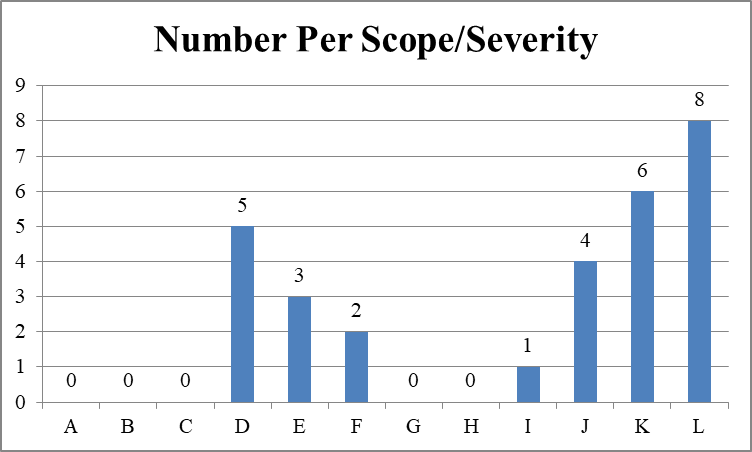
Expanding
the 20% sample (18 times five) still means that only 90 facilities were likely
cited with an immediate jeopardy deficiency in infection prevention and control
since January 2020.
The
Center looked at the sample of 25 nursing facilities with infection control
deficiencies on Nursing Home
Compare. One facility did not appear on Nursing Home Compare at all
and another facility is a Special Focus Facility and, therefore, does not have
star ratings.
Health ratings of 23 nursing facilities cited with infection
control deficiencies
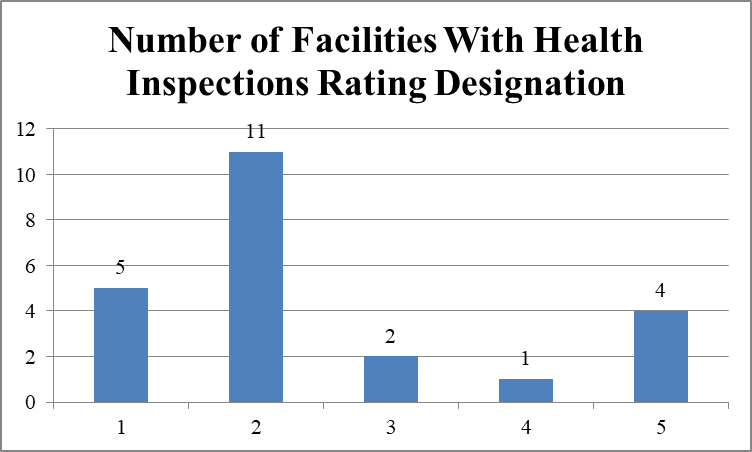
Facilities
identified in QCOR as having immediate jeopardy deficiencies in infection
control had poor records for quality of care. Sixteen of 23 facilities
(69.6%) have one or two stars in health inspections; five of 23 facilities
(21.7%) have four or five stars.
Staffing ratings of 23 nursing facilities cited with infection
control deficiencies
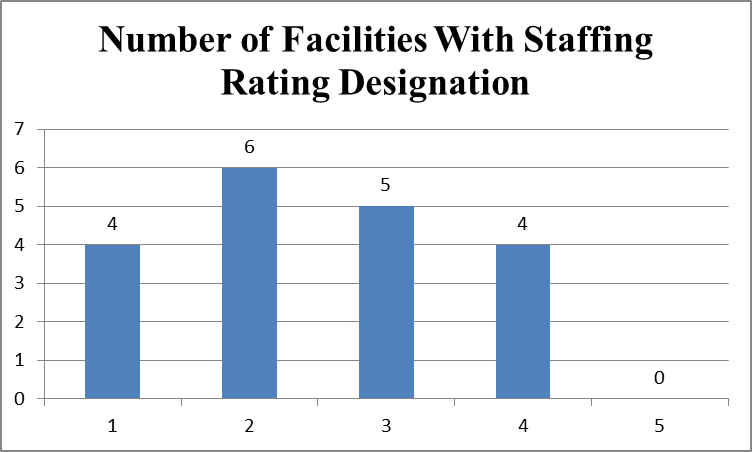
Facilities
identified in QCOR as having immediate jeopardy deficiencies in infection
control also had poor staffing levels. Ten of 23 facilities (43.5%) have
one or two stars in staffing; four of 23 facilities (17.4%) have four stars in
staffing; four facilities do not have staffing ratings. No facility has
five stars in staffing.
Quality measure ratings of 23 nursing facilities cited with
infection control deficiencies
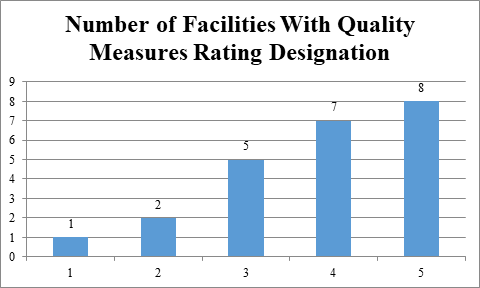
Facilities
identified in QCOR as having immediate jeopardy deficiencies in infection
control nevertheless self-report resident assessment data that makes them look
good in the quality measure domain. Fifteen of 23 facilities (65.2%) have
four or five stars in quality measures. These data document, again, that
facilities’ largely self-reported quality measure data are inconsistent with
the health inspection and staffing measures and make facilities look much
better than they should.
Overall ratings of 23 nursing facilities cited with infection
control deficiencies
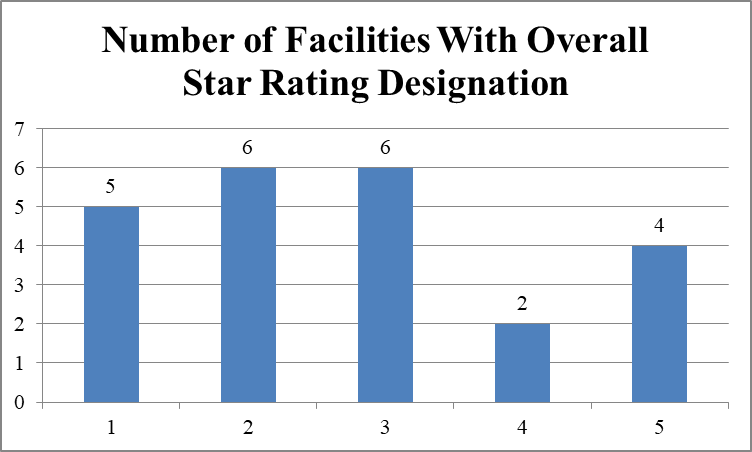
Eleven
of 23 facilities (47.8%) have one or two stars in quality measures; six of 23
facilities (26.1%) have four or five stars in quality measures.
Penalty History
Eight
of the 24 facilities (33.3%) had civil money penalties imposed in the prior
three years, according to Nursing
Home Compare; the fines averaged $56,692.13 and totaled
$453,537. The Special Focus Facility was fined $166,183. Sixteen of
the 25 facilities (66.7%) had no fines in the prior three years.
A
total of six denials of payment for new admissions (DPNA) had been imposed at
the 24 facilities in the prior three years. The Special Focus Facility
had three DPNAs; one facility had two DPNAs; and one facility had one DPNA.
QCOR and CMPs
QCOR
also separately identifies civil money penalties (CMPs) that are imposed for
infection prevention and control deficiencies. Comparing the QCOR
deficiency data with the QCOR CMP data, the Center found that 14 of the 25
facilities (56%) with infection control deficiencies had CMPs. Thirteen
facilities had per day CMPs imposed, totaling $1,348.397.75; one facility had
two per instance CMPs, totaling $21,768.50. Nursing Home Compare does not report CMPs for
facilities that are appealing the deficiencies and CMPs.
- Of the 14 facilities with immediate jeopardy deficiencies in
infection control, 11 had CMPs imposed and three did not.
- Of the seven facilities with only non-jeopardy deficiencies
in infection control, three had CMPs imposed and four did not.
QCOR and CMS’s Fifth Cumulative Date Release of Focused Infection
Control Surveys
On
September 30, CMS made available on Nursing
Home Compare its fifth cumulative release of focused infection
control surveys, covering the period January-August 2020.[4] The Center compared the 75
facilities reported on Nursing
Home Compare as having been cited with infection control
deficiencies with the 25 facilities reported in the QCOR sample and found only
11 facilities listed in both databases.
Discussion/Conclusion
QCOR
is inaccurate in its reporting of infection prevention and control
deficiencies. While QCOR indicates that 384 immediate jeopardy infection
control deficiencies had been cited since January 2020, the Center for Medicare
Advocacy’s review of a 20% sample of the 384 deficiencies (i.e., 59
deficiencies) found that only 25 of 59 facilities were actually cited with an
infection control deficiency. Expanding the 20% sample means that 125
facilities have been cited with an infection control deficiency. But only
18 of the 25 facilities were cited with an immediate jeopardy deficiency in
infection control. Expanding that 20% sample means that 90 facilities
have been cited with an immediate jeopardy infection control deficiency since
January 2020, half the 180 facilities cited by CMS in August.
Enforcement
of these deficiencies appears limited. QCOR data also show that only 11
of the 18 facilities (61%) cited with immediate jeopardy infection control
deficiencies had CMPs imposed. It is possible that more CMPs have been
imposed. Since QCOR reports only CMPs that are “final,” any CMPs that
facilities have appealed are not listed.
Also
troubling is the limited overlap between CMS’s two public databases, QCOR and Nursing Home Compare.
Of the 18 facilities in the Center’s sample with immediate jeopardy
deficiencies in infection control identified in QCOR, only ten facilities are
reported in Nursing Home
Compare.
Infection
control deficiencies are rarely cited and, even if cited, they are not cited as
immediate jeopardy and are not enforced. Proper enforcement could prevent
unnecessary deaths.
___________________
[1] CMS, “Trump
Administration Has Issued More Than $15 Million in Fines to Nursing Homes
During COVID-19 Pandemic” (Press Release, Aug. 14, 2020), https://www.cms.gov/newsroom/press-releases/trump-administration-has-issued-more-15-million-fines-nursing-homes-during-covid-19-pandemic.
[2] CMA, “Responding to CMS Announcement on Nursing Home Enforcement
– Infection Control Deficiencies in Nursing Facilities: QCOR Data” (CMA Alert,
Aug. 20, 2020).
[3] The Center analyzed ## 1, 6, 11, and so on.
[4] CMA, “Special Report: CMS Releases Fifth Cumulative List of
Focused Infection Control Surveys” (CMA Alert, Oct. 8, 2020), https://medicareadvocacy.org/special-report-cms-releases-fifth-cumulative-list-of-focused-infection-control-surveys/.
No comments:
Post a Comment